Connect With Us
Featured Articles

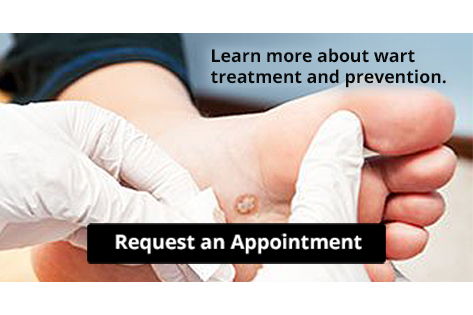
How Are Foot Warts Treated?
Most plantar warts, warts that develop on the bottom of the foot, go away after months or years on their own. However, as these warts can cause pain and discomfort, and because they are contagious and can spread easily, a doctor may recommend or prescribe various treatments and at home care techniques to help you find relief. To treat a foot wart, your doctor may prescribe a topical medication, which you must use exactly as prescribed for best results. You may also take an over-the-counter pain medication to reduce pain from the wart. Wearing comfortable shoes and socks, and padding the wart by wearing a doughnut-shaped felt or moleskin bandage, may also help relieve pain by reducing pressure placed on the wart. For the best treatment options, consult with a podiatrist today.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. Thong V. Truong from California. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Chico, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Are Plantar Warts?
Plantar warts are described as small growths that appear on the heels or other areas of the feet that bear a large amount of weight. The pressure in these areas causes plantar warts to hide behind thick layers of skin called calluses. In most cases, plantar warts are not a serious health issue, and they usually go away without treatment. However, it is still important be mindful of them.
Plantar warts are caused by infections with human papillomavirus (HPV) in the outer layer of skin on the soles of the feet. The plantar warts then develop when the virus enters the body through weak spots at the bottom of the feet, such as tiny cuts and breaks. Plantar warts are not guaranteed for all who encounter the virus. Everyone responds differently to the affects of HPV.
Plantar warts are most common in the following groups: children and teenagers, people with weakened immune systems, people with history of plantar warts, and people who walk barefoot. Exposure to HPV is common in environments such as locker rooms or pool areas.
One of early signs to look out for is a callus, since many plantar warts hide behind them. You can also locate these warts by looking for small, fleshy, rough, grainy growths near the base of the toes and the heel. Early signs of plantar warts are shown by black pinpoints, which are small, clotted blood vessels. Lesions that interrupt normal lines and ridges in the skin of your foot may also be a sign of plantar warts. Any feeling of pain while walking or standing can also be a symptom of plantar warts.
Although most cases are not serious, some conditions may require a visit to your podiatrist. If you are uncertain that your lesion is a wart, if you have diabetes, or if you are experiencing bleeding, you may need to see a seek professional treatment. Your doctor may offer treatments such as prescribing stronger peeling medicine or using cryotherapy by applying liquid nitrogen to the wart. More serious cases may require minor surgery or laser treatment.
There are simple solutions available to help prevent plantar warts. One common task is to avoid walking barefoot in swimming pool areas and locker rooms, as this is where HPV is commonly present. Keeping your feet clean and dry, while changing shoes and socks daily can also help prevent future plantar warts. If you know someone who has plantar warts, it is important to avoid direct contact with their warts. You should also refrain from picking or scratching your wart if you happen to develop one.
What Should I Do if I Have Athlete's Foot?
 Tinea pedis, or Athlete’s foot as it is more commonly known, is a fungal infection of the skin and feet. It typically affects the spaces between the toes and is characterized by cracked, scaly skin. This infection is contagious and can be spread through contact with infected skin flakes or through contact with fungi in damp areas, such as public swimming pools. If you find yourself with athlete’s foot, it is important to keep the feet clean, dry, and cool, as the fungus thrives and multiplies in warm, moist environments. You should also avoid public swimming pools, public showers, and foot baths. Wear sandals if possible, or air out your shoes by alternating them every 2-3 days. Avoid wearing socks made from fabrics like nylon, which do not dry easily. Finally, follow your doctor’s prescribed treatments, which can include topical or oral antifungal medications. If you think that you may have athlete’s foot, it is suggested that you seek the care of a podiatrist.
Tinea pedis, or Athlete’s foot as it is more commonly known, is a fungal infection of the skin and feet. It typically affects the spaces between the toes and is characterized by cracked, scaly skin. This infection is contagious and can be spread through contact with infected skin flakes or through contact with fungi in damp areas, such as public swimming pools. If you find yourself with athlete’s foot, it is important to keep the feet clean, dry, and cool, as the fungus thrives and multiplies in warm, moist environments. You should also avoid public swimming pools, public showers, and foot baths. Wear sandals if possible, or air out your shoes by alternating them every 2-3 days. Avoid wearing socks made from fabrics like nylon, which do not dry easily. Finally, follow your doctor’s prescribed treatments, which can include topical or oral antifungal medications. If you think that you may have athlete’s foot, it is suggested that you seek the care of a podiatrist.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Dr. Thong V. Truong from California. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our office located in Chico, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Athlete's Foot
Athlete’s foot is an extremely contagious infection caused by a fungus that results in itching, burning, dry, and flaking feet. The fungus that causes athlete’s foot is known as tinea pedis and thrives in moist, dark areas such as shower floors, gyms, socks and shoes, commons areas, public changing areas, bathrooms, dormitory style houses, locker rooms, and public swimming pools. Athlete’s foot is difficult to treat as well because of the highly contagious and recurrent nature of the fungus.
Tinea is the same fungus that causes ringworm, and is spread by direct contact with an infected body part, contaminated clothing, or by touching other objects and body parts that have been exposed to the fungus. Because the feet are an ideal place for tinea to grow and spread, this is the most commonly affected area. It is, however, known to grow in other places. The term athlete’s foot describes tinea that grows strictly on the feet.
The most commonly infected body parts are the hands, groin, and scalp, as well as the feet. Around 70% of the population suffer from tinea infections at some point in their lives, however not all of these cases are athlete’s foot. Just like any other ailment, some people are more likely to get it than others, such as people with a history of tinea infections or other skin infections, both recurring and non-recurring ones. The extent to which a person experiences regrowth and recurrent tinea infections varies from person to person.
Sometimes people will not even know that they are infected with tinea or that they have athlete’s foot because of a lack of symptoms. However, most experience mild to moderate flaking, itching, redness, and burning. However, some of the more severe symptoms include cracking and bleeding skin, intense itching and burning, pain while walking or standing, and even blistering.
Because of the recurring nature of the tinea fungus and the athlete’s foot it causes, the best way to treat this condition is with prevention. You can take some preventative measures such as wearing flip flops or sandals in locker rooms and public showers to reduce contact with the floor. It also helps to keep clean, dry feet while allowing them to breathe. Using powders to keep your feet dry is a good idea, as well as keeping your feet exposed to light and cool air, to prevent the growth of tinea. If you do happen to get athlete’s foot, opt for using topical medicated creams, ointments or sprays. These treatments help eliminate and prevent it from coming back.
Ways to Prevent Hammertoe
Hammerto e is a deformity of the toes that causes the small toes to bend at the joint. If left untreated, hammertoes can be permanent. Common signs of hammertoe include curling toes, thickening of the skin on the affected toe, trouble finding shoes that fit correctly, and pain. One of the leading causes of hammertoe is poor fitting shoes. Avoid shoes that have a narrow and pointed toe, that are too tight, or that have a high heel. Shoes that have wide toe boxes and are roughly a half inch longer than your longest toe are generally best to reduce the risk of hammertoe. A proper diagnosis and treatment plan for hammertoe will require visiting a podiatrist, so if you believe that you are suffering from hammertoe, consult with a podiatrist as soon as possible.
e is a deformity of the toes that causes the small toes to bend at the joint. If left untreated, hammertoes can be permanent. Common signs of hammertoe include curling toes, thickening of the skin on the affected toe, trouble finding shoes that fit correctly, and pain. One of the leading causes of hammertoe is poor fitting shoes. Avoid shoes that have a narrow and pointed toe, that are too tight, or that have a high heel. Shoes that have wide toe boxes and are roughly a half inch longer than your longest toe are generally best to reduce the risk of hammertoe. A proper diagnosis and treatment plan for hammertoe will require visiting a podiatrist, so if you believe that you are suffering from hammertoe, consult with a podiatrist as soon as possible.
Hammertoes can be a painful condition to live with. For more information, contact Dr. Thong V. Truong of California. Our doctor will answer any of your foot- and ankle-related questions.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the muscles, tendons, or ligaments that normally hold the toe straight. It can be caused by the type of shoes you wear, your foot structure, trauma, and certain disease processes.
Symptoms
- Painful and/or difficult toe movement
- Swelling
- Joint stiffness
- Calluses/Corns
- Physical deformity
Risk Factors
- Age – The risk of hammertoe increases with age
- Sex – Women are more likely to have hammertoe compared to men
- Toe Length – You are more likely to develop hammertoe if your second toe is longer than your big toe
- Certain Diseases – Arthritis and diabetes may make you more likely to develop hammertoe
Treatment
If you have hammertoe, you should change into a more comfortable shoe that provides enough room for your toes. Exercises such as picking up marbles may strengthen and stretch your toe muscles. Nevertheless, it is important to seek assistance from a podiatrist in order to determine the severity of your hammertoe and see which treatment option will work best for you.
If you have any questions, please feel free to contact our office located in Chico, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Hammertoes?
Hammertoes are painful deformities that frequently form on the second, third, or fourth toe. The condition is often caused by an issue in foot mechanics. This can be caused by the person’s specific gait or the manner in which they walk, or by shoes that do not comfortably fit the deformity. Hammertoes can be formed after wearing shoes that are too narrow or short for the foot or have excessively high heels. Shoes that are not properly sized will force the toes into a bent position for long periods of time. This can cause the muscles to shorten and toes to bend into the deformity of a hammertoe.
Hammertoe can also be caused by complications from rheumatoid arthritis, osteoarthritis, trauma to the foot, heredity, or a cerebral vascular accident. Pain and difficult mobility of the toes, deformities, calluses, and corns are all symptoms of a hammertoe.
Someone who suspects they have the symptoms of a hammertoe should consult with a physician—particularly a podiatrist. Podiatrists diagnose and treat complications of the foot and ankle. If the podiatrist discovers that the affected toes are still flexible, treatment for the hammertoe may simply involve exercise, physical therapy, and better-fitting shoes. Treatment for hammertoes typically involves controlling foot mechanics, such as walking, through the use of customized orthotics.
For more serious cases in which the toes have become inflexible and rigid, surgery may be suggested. During the operation, the toe would receive an incision to relieve pressure on the tendons. A re-alignment of the tendons may then be performed by removing small pieces of bone to straighten the toe. In some cases, the insertion of pins is needed to keep the bones in the proper position as the toe heals. The patient is usually allowed to return home on the same day as the surgery.
If surgery is performed to repair a hammertoe, following the postoperative directions of your doctor is essential. Directions may include several stretches, picking up marbles with your toes, or attempting to crumple a towel placed flat against your feet. Wear shoes that have low heels and a wide amount of toe space to maintain comfort. Closed-toe shoes and high heels should be avoided. Shoes with laces allow the wearer to adjust how fitted he or she may want the shoes to be and also allow for greater comfort. To provide adequate space for your toes, select shoes that have a minimum of one-half inch of space between the tip of your longest toe and the inside of the shoe. This will also relieve pressure on your toes and prevent future hammertoes from forming.
Other preventative measures that can be taken include going shopping for new shoes in the middle of the day. Your feet are its smallest in the morning and swell as the day progresses. Trying on and purchasing new shoes midday will give you the most reliable size. Be sure to check that the shoes you purchase are both the same size. If possible, ask the store to stretch out the shoes at its painful points to allow for optimum comfort.
Arthritis Can Cause Pain in the Feet and Ankles
Defining and Treating Plantar Fasciitis
 One common source of heel pain is plantar fasciitis, which occurs when the plantar fascia, the tissue connecting the heel to the bottom of the foot, is inflamed. Common symptoms of plantar fasciitis include sharp heel pain, pain after resting, heel tenderness, pain while flexing, and tingling or burning in the bottom of the foot. Upon experiencing symptoms, it is important to visit a podiatrist. During the exam, a podiatrist will examine any swelling, tenderness and pain points. After the examination, your podiatrist will suggest a variety of treatment options that can include rest, orthotics, stretching, icing, and massages. Medicine may also be prescribed. If you think that you are suffering from plantar fasciitis, it is suggested that you visit a podiatrist.
One common source of heel pain is plantar fasciitis, which occurs when the plantar fascia, the tissue connecting the heel to the bottom of the foot, is inflamed. Common symptoms of plantar fasciitis include sharp heel pain, pain after resting, heel tenderness, pain while flexing, and tingling or burning in the bottom of the foot. Upon experiencing symptoms, it is important to visit a podiatrist. During the exam, a podiatrist will examine any swelling, tenderness and pain points. After the examination, your podiatrist will suggest a variety of treatment options that can include rest, orthotics, stretching, icing, and massages. Medicine may also be prescribed. If you think that you are suffering from plantar fasciitis, it is suggested that you visit a podiatrist.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Thong V. Truong from California. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Chico, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.